Pressure sores, also known as decubitus ulcers, are a fairly common problem among residents living at skilled nursing facilities. The challenge for nursing homes is two-fold. First, how to prevent pressure sores from occurring in the first place, and secondly, how to promote healing in situations when a resident is admitted with a pressure sore from the start. This article is meant to provide information and advice to both the clinical teams at nursing homes and the families of residents who reside in them.
What are pressure sores and how to do they develop?
A pressure sore is an area of the skin that is broken (ulcerated) due to the blood supply being cut off from lack of oxygen to it. Patients are prone to developing pressure sores when sitting or lying in bed for a long period of time. Wherever there's a bony prominence, for example, the sacral area, heels or elbows, and pressure is applied, just as would happen when somebody's lying in bed over time, it ultimately can impair circulation and lead to skin breakdown.
What Can a Nursing Home Do to Prevent a Pressure Sore upon Admission?
 To prevent a wound from turning into a potentially harmful pressure sore, it is recommended that every resident have a would assessment upon admission to a nursing facility. A wound assessment would be an evaluation of the entire body in search of wounds, their characteristics, and, if previously documents, their history.
To prevent a wound from turning into a potentially harmful pressure sore, it is recommended that every resident have a would assessment upon admission to a nursing facility. A wound assessment would be an evaluation of the entire body in search of wounds, their characteristics, and, if previously documents, their history.
There are also pressure relieving mattresses and heal elevators that can act as preventive care. It’s likely a resident might develop pressure sores on their heels, so a nurse can even roll up a towel and put it behind the ankle just to keep the pressure removed where a heel would otherwise be in contact with the sheets.
What Should a Nursing Home do if a Resident already has a Pressure Sore?
There are several important steps a nursing home can take to prevent pressure sores from getting worse, even potentially deadly. The healing process lies within a nursing home’s wound care protocol. For example, a competent protocol would include daily skin inspections, especially at the time of each nurse’s shift change. Not only does it allow for several inspections per day, but it allows multiple clinicians to have a fresh set of eyes on the sore. Also, cleaning and applying fresh bandages several times per day decreases the risk of infection.
If a pressure sore gets below the first layers of skin, know as the epidermis, then there is a good chance that a surgical procedure known as a debridement is necessary to remove rotten and dead tissue around the sore. That is why it is important to have a physical checkup scheduled once a pressure sore is detected.
What are the 4 Stages of Pressure Sores?
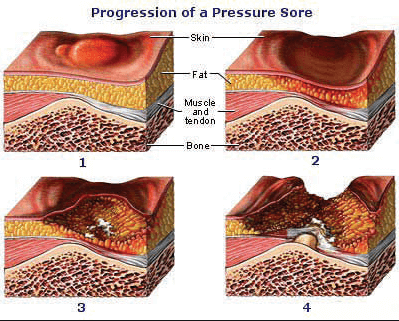 There are four stages of pressure sores; stage four being a most serious and potentially deadly.
There are four stages of pressure sores; stage four being a most serious and potentially deadly.
Stage One: this is mildest stage in which a sore on the top layer of the skin occurs. Symptoms included red or discolored skin, warmer temperature, and mild pain, burning and/or itching may occur. At this stage the sore has not penetrated to the soft tissue, muscle or bone.
Stage Two: the sore becomes an open wound. The top layer of skin has been broken and the sore hits deeper layers of the skin. It has not yet hit the soft tissue, muscle or bone. The sore takes on the shape of an ulcer or blister. It also can contain fluid.
Stage Three: the sore travels deeper and hits the soft tissue below the skin. Bone, tendon and muscle are not visible. There could be puss and/or greenish drainage. A fever could develop.
Stage Four: the sore is now at its deepest and is hitting the soft tissue, muscle, tendon, and bone. More than likely infection has occurred. Puss and drainage are probably present.
Conclusion
It’s essential that the clinical team does everything possible to prevent skin breakdown which results in pressure sores or decubitus ulcer. When a resident already has a pressure sore the facility is responsible to do everything conceivable to promote its healing, and that starts with a proper wound care assessment by a trained wound physician or nurse. It should also be stated that adequate documentation is always necessary to demonstrate the facility has done everything possible to prevent a pressure sore. Having a medical history of the pressure increases probability of proper treatment and healing.


Comments